Understanding Postural Orthostatic Tachycardia Syndrome (POTS)
For millions of Americans who suffer from on-again, off-again dizzy spells, nausea and chest pains, they’re just as likely to be told by their doctor that they’re living with a psychological disorder — something akin to anxiety or depression — than a physical medical condition.
Seriously? Your symptoms, which may include fatigue, insomnia, brain fog and headaches, are reflective of a psychological issue rather than a commonplace physical ailment that affects millions of Americans each year? What could be more damaging to the soul than hearing “it’s all in your head”?
You’re certain such a diagnosis is not the case, but nobody with a medical credential will listen to you or take your concerns seriously. The only comfort you can draw from this information is that millions of people in this country suffer from a disorder with those very same symptoms. It’s called postural orthostatic tachycardia syndrome or POTS.
Never heard of it?
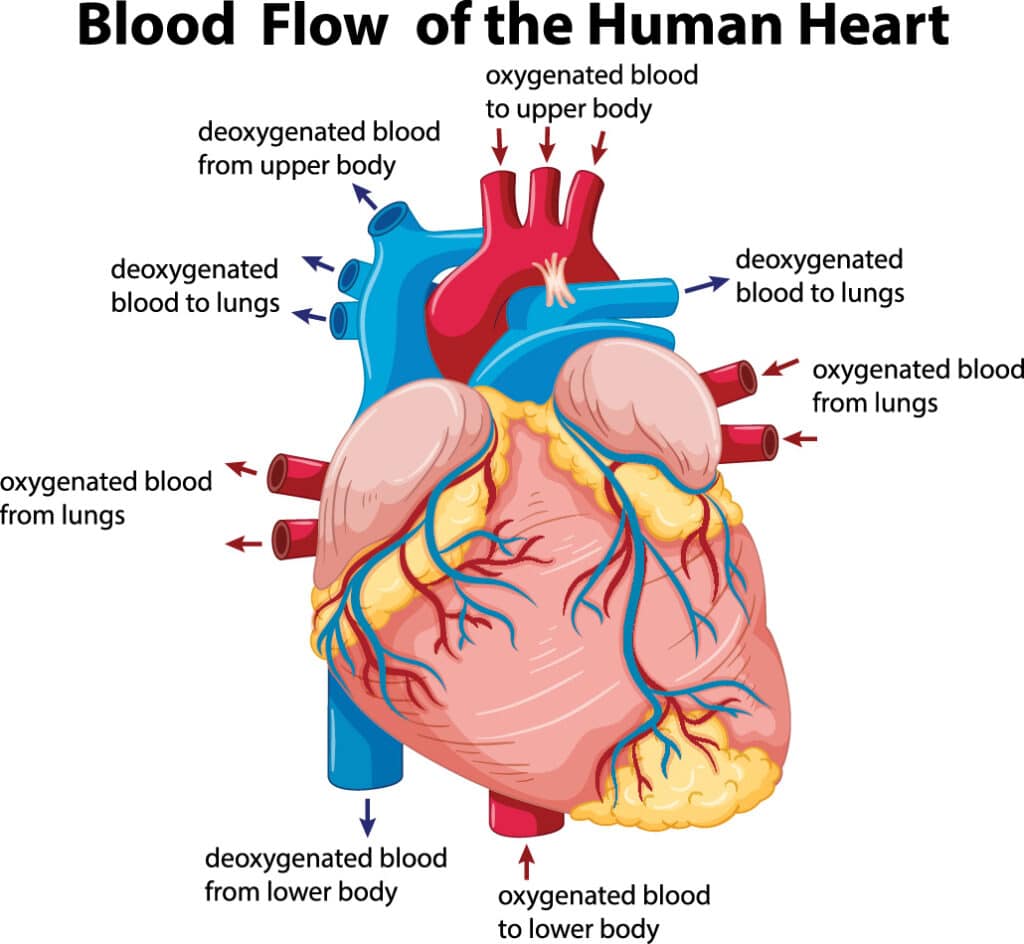
POTS is a group of disorders where smaller volumes of blood return to the heart after you stand up from a prone position. That’s the most obvious symptom, but few doctors can point a finger at it and diagnose it as POTS.
POTS is a form of dysautonomia — an encompassing medical term for conditions caused by a dysfunction of the autonomic nervous system. This condition affects the flow of blood, causing dizziness when standing up. When you stand up, much of the blood in your body drains to the lower parts of the body, but your autonomic nervous system — which operates on an involuntary reflex — normally makes sure some of that blood remains circulating in the upper body. Those afflicted with POTS often experience dizziness when standing, as well as frequent fatigue, which greatly diminishes daily activities.
Who is most likely to be affected by POTS?
Researchers point to women in their teens through 30s. And while dizziness is a primary symptom of POTS, additional signs can include headaches, stomach pains, nausea, tremors, a racing heart, pain in the chest, shortness of breath, insomnia, and even bladder issues.
Often referred to as “the fainting disease” or “the invisible illness,” a diagnosis of POTS does not rely on dizziness as a major player in a reliable diagnosis of the problem.
Diagnosing and treating postural orthostatic tachycardia syndrome
The doctors and staff here at Restoration Healthcare have a great deal of experience with postural orthostatic tachycardia syndrome and can diagnose the condition with a noninvasive test that takes about 20 minutes to complete and features sophisticated software connected by probes to your body that send signals to a computer for analysis.
As a result of such testing, we can accurately determine a diagnosis and a treatment plan. Such a diagnosis, however, is made all the more difficult for patients who suffer from Lyme disease, human granulocytic anaplasmosis (HGA), and babesiosis — different diseases, but all borne by the same family of tick. As a result, the Lyme/POTS patient that arrives at our office is in need a practitioner who is experienced in treating Lyme and not just POTS — and that’s where our own Medical Director, Dr. Sunny Raleigh, comes in to the picture. Dr. Raleigh is one of Southern California’s top Lyme disease detectives and treatment specialists.
Treating patients with POTS
And what is our “Rx” when it comes to POTS? Accurate monitoring and coaching in lifestyle changes is the key. Due to fatigue, POTS patients often have low reserves for exercise, so we monitor you to determine how much you can handle and then “dose” you accordingly.
We also identify any foods or substances consumed on a regular basis that might add or prompt the syndrome. For example, gluten might turn out to be a major factor, so testing the cross reactivity of auto immune issues is important in order to eliminate those substances from your diet.
We approach the search for a diagnosis much as a detective goes about seeking clues to a crime — by examining all possible causes and contributions rather than depending on one set protocol. Call us scientific snoops, if you will, but be confident that we will find the proper diagnosis and prescribe the proper solution to postural orthostatic tachycardia syndrome.