Understanding Hypermobile Ehlers-Danlos Syndrome (EDS)

Surprising Challenges of Hypermobile Ehlers-Danlos Syndrome and EDS Symptoms: Beyond Flexibility
Flexibility is a good thing, right? Nobody wants tight muscles and stiff joints. But is it possible to be too flexible? If you ask people with hypermobile Ehlers-Danlos Syndrome, you’ll get an answer that might surprise you — yes, it is possible to be too flexible.
Imagine popping your knee while walking across the street or dislocating your shoulder trying to lift a cup of coffee (in extreme cases). Or maybe you don’t need to imagine it. Maybe you or someone you know is living with hypermobile Ehlers-Danlos Syndrome (pronounced A-lurz DAN-loss SIN-drome).
For the uninitiated, Ehlers-Danlos Syndromes (EDS) is a group of 13 genetic disorders related to the body’s connective tissues — primarily the skin, joints, and blood vessel walls. Symptoms vary according to the specific syndrome, but Hypermobile EDS (hEDS), which accounts for about 80–90 percent of all cases, is characterized primarily by excessively flexible joints and thin, stretchy skin.
Thanks to a few celebrities, namely Lena Dunham, Jameela Jamil, Sia, and Halsey, awareness of Ehlers Danlos syndrome is growing, and that’s a good thing because knowledge can help those who live with this condition avoid unnecessary injuries and can lead to better health outcomes.
In this post, we provide the information and guidance you need to understand hEDS symptoms and make well-informed health decisions if you’re living with this condition.
Hypermobile Ehlers-Danlos Syndrome (hEDS) Symptoms
Hypermobile Ehlers-Danlos Syndrome (hEDS) and hypermobility spectrum disorders are characterized by overly flexible joints. People with these conditions are at risk of injury because their joints are too flexible.
Patients with EDS disease and heds syndrome have inherited flaws in the function, strength, and structure of their collagen. Collagen is an important protein that provides structural support in your blood vessels, ligaments, skin, cartilage, tendons, and organs.
In addition to increasing one’s risk of injury, the following symptoms also plague people who have this disorder:
- Frequent joint dislocation (partial or full)
- Chronic joint or bone pain
- Chronic fatigue
- Mast cell activation
- Poor circulation
- Early onset arthritis
- Atrophic scarring (sunken or depressed scars with well-defined borders)
- Postural orthostatic tachycardia syndrome (POTS) — a condition that causes an increased heart rate along with feelings of dizziness or fainting episodes
- Bladder/urinary dysfunction
- Digestive and gastrointestinal issues — abdominal cramping, bloating, loose stools, constipation
- Anxiety
- Disturbed sleep
- Depression
- Mitral valve prolapse in the heart
- Aortic root dilation
- Uterine, rectal, or bladder prolapse
- Varicose veins
- Osteoporosis
- Skin that stretches, tears, and bruises easily
Gymnasts, ballerinas, dancers, contortionists, and swimmers (especially those who’ve mastered the butterfly stroke), can use this added flexibility to their advantage, which is a good thing. Until it’s not. Over time, hEDS takes its toll on the joints, leading to painful injuries. What’s worse is when surgery is performed to repair the injury without accommodating for hEDS, it does more harm than good.
Hypermobility Diagnosis
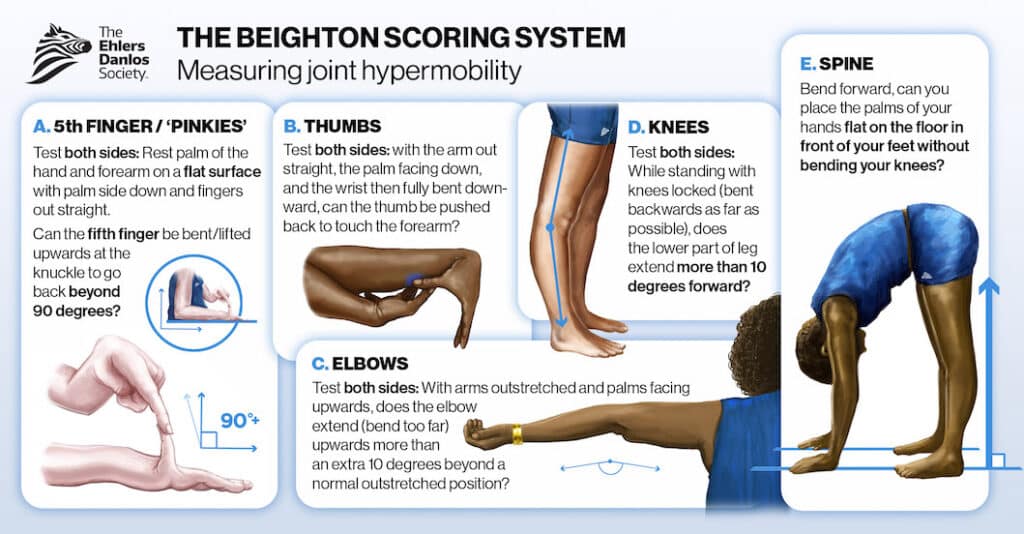
If you suspect you have hypermobility, be sure to report it to your doctor, who should perform a physical exam to check your flexibility. Your experienced integrative physicians should also examine your skin and eyes, listen to your heart, and order a blood test to check for any signs of EDS. If your doctor doesn’t suggest the possibility of EDS, ask.
If you’re merely far more flexible than normal, you may be diagnosed with simple hypermobility. If you have additional symptoms, such as dizziness when you stand up, chronic joint pain, fatigue, and abnormal scarring, you’re more likely to be diagnosed as having hypermobile EDS and possibly other related conditions. EDS can affect your eyes, blood vessels, and various organs, including your heart, kidneys, and spleen. It can be life-threatening. Ask your doctor about testing for these related conditions.
Living with Hypermobility
Hypermobility isn’t a condition that can be cured, but you can be proactive in managing it. Focus your efforts on the following four areas:
- Exercise
- Lifestyle
- Psychological/emotional support
- Additional treatments
Exercise
Physical activity can help strengthen your muscles and provide your joints with the support they need. But don’t overdo it. Here are a few suggestions:
- Engage in activities that build strength without subjecting your joints to sudden movements. Walking, bicycling, and water aerobics are great. Avoid activities that stress the joints, such as golf and tennis.
- Don’t overstretch.
- Tape or brace your overly flexible joints to prevent injuries.
- Practice tai chi or qi gong, which uses slow, controlled movements to tone muscles and strengthen joints.
- Practice good posture.
Lifestyle
Lifestyle changes help to build and maintain health overall, including joint health:
- Eat a healthy diet, mostly whole foods and mostly plant-based.
- Drink enough water.
- Establish a healthy sleep routine to ensure that you’re getting 7–8 hours of sleep per night (the body repairs itself during sleep).
- Maintain a healthy weight.
- Don’t smoke or vape.
- Don’t drink alcohol in excess (no more than one or two drinks daily).
Psychological/emotional support
Living with EDS can be psychologically and emotionally draining, so pay attention to your mood and take the following steps to maintain your mental health and well-being:
- Try to reduce stress as much as possible.
- Maintain a sense of purpose through work, volunteering, hobbies, and other activities.
- Explore natural ways to manage stress and reduce pain — for example, yoga, mindfulness training, and massage.
- Discuss your feelings with friends, family members, or a therapist. People with hEDS sometimes feel as though they’re a burden to others. Talking about it can help ease those concerns.
Other treatments for hEDS Symptoms
To alleviate some of the pain and discomfort of hEDS, try the following:
- Apply heat or cold to reduce pain.
- If you feel dizzy or light-headed or you faint frequently, have your doctor check for postural orthostatic tachycardia syndrome (POTS). Wearing compression stockings and getting more fluids may help, but dietary changes may also be necessary — for example, eliminating gluten.
- Inform your doctors, dentist, surgeons, and physical therapists that you have hypermobility treatments so that they can adjust their treatment accordingly. It is important to be your own advocate and inform medical professionals about your condition. Your healthcare team needs to factor EDS into your recovery, which might take longer than expected.
How Restoration Healthcare Can Help with EDS Symptoms
When you’re living with hypermobility, having someone on your medical team who fully understands the condition can lead to much better treatment outcomes. Here’s how we can help:
- Diagnose hypermobility, hEDS, and other EDS conditions.
- Diagnose and treat other underlying health conditions that may be contributing to the pain and inflammation.
- Educate about not overstretching, because that can lead to long-term joint damage.
- Provide diet and lifestyle guidance to support overall health.
- Consult with orthopedic doctors and surgeons to ensure that treatments are handled in the best way possible. For example, if a surgical procedure requires the use of screws, they must be done differently to ensure that they don’t tear through the bone. We’ve seen a case when a patient with a dislocated shoulder had to have it surgically repaired four times because the surgeon failed to make accommodations for the patient’s EDS.
- Refer patients to, and consult with, physical therapists to ensure that their therapy protocols account for their patients’ EDS. Some physical therapists are specialized to provide a type of physical therapy that acknowledges and addresses the special needs of those with EDS.
Depending on the degree of hypermobility you’re experiencing, it may or may not be a major concern, but you should have it checked out. Early diagnosis and intervention can lead to significantly better outcomes while preventing joint injuries and delaying or even preventing the onset of arthritis.
If you’re in or near Southern California or plan to visit the area, contact us to schedule an initial consultation with Restoration Healthcare. Otherwise, we strongly encourage you to consult with a functional and integrative medical practice near you that has experience diagnosing and treating hypermobility and EDS. You really need someone on your treatment team who understands these conditions to advocate for you and serve in a consultative capacity to ensure that you’re receiving treatment that improves your condition without making it worse.
– – – – – – – – – – – –
Disclaimer: The information in this blog post about Hypermobile Ehlers-Danlos Syndrome is provided for general informational purposes only and may not reflect current medical thinking or practices. No information contained in this post should be construed as medical advice from the medical staff at Restoration Healthcare, Inc., nor is this post intended to be a substitute for medical counsel on any subject matter. No reader of this post should act or refrain from acting on the basis of any information included in, or accessible through, this post without seeking the appropriate medical advice on the particular facts and circumstances at issue from a licensed medical professional in the recipient’s state, country or other appropriate licensing jurisdiction.